Peripheral Vascular Disease (PVD), also known as Peripheral Arterial Disease (PAD), is a common yet serious condition that affects the blood vessels outside the heart and brain, particularly those that supply blood to the limbs. This chronic disease can lead to pain, numbness, and, if untreated, significant complications. Understanding PVD, its symptoms, and the risk factors is crucial for effective management and prevention.
What is Peripheral Vascular Disease?
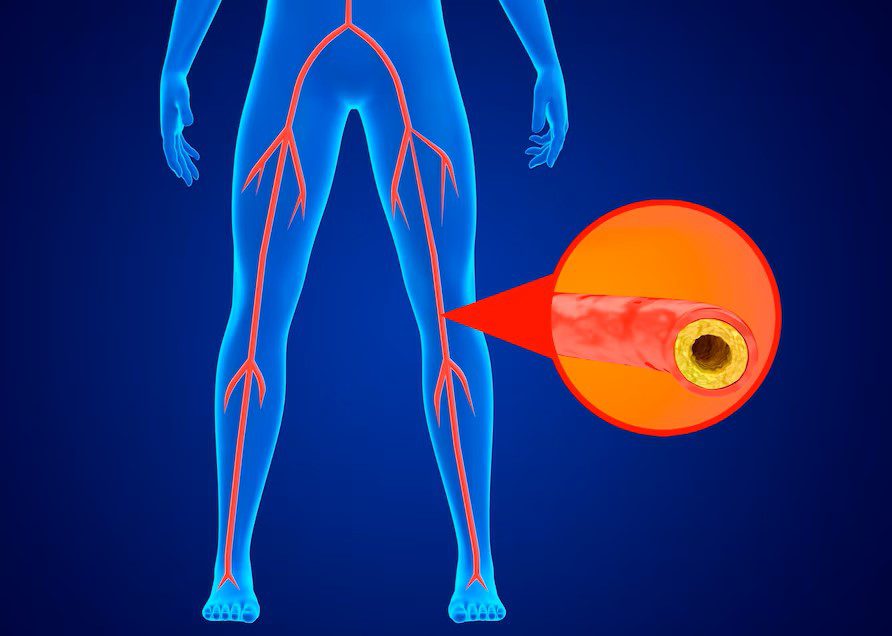
Peripheral Vascular Disease occurs when the arteries in the legs, arms, and other areas outside the heart and brain become narrowed or blocked. This obstruction reduces blood flow and oxygen delivery to the affected areas, often resulting in pain, discomfort, or other symptoms. The reduced circulation can lead to tissue damage, ulcers, and in severe cases, even limb amputation.
Symptoms of Peripheral Vascular Disease
PVD symptoms can vary in severity, but the most common include:
- Leg Pain (Claudication): Pain or discomfort in the legs, especially during physical activity, which eases with rest.
- Numbness or Weakness: A sensation of numbness or weakness in the legs or arms, often exacerbated by movement.
- Coldness in Limbs: Persistent coldness in the legs or feet, even when the rest of the body feels warm.
- Sores or Ulcers: Slow-healing sores or ulcers on the legs or feet, which can become infected.
- Weak or Absent Pulse: A noticeable decrease in the pulse in the legs or feet.
- Skin Changes: Changes in skin color (pale, bluish, or reddish) or texture in the affected limbs.
Risk Factors for Peripheral Vascular Disease
Understanding and managing risk factors is key to preventing and controlling PVD. Major risk factors include:
- Age: The risk of developing PVD increases as you age, particularly after 50.
- Smoking: Smoking significantly damages blood vessels and is one of the strongest risk factors for PVD.
- Diabetes: High blood sugar levels can damage blood vessels, increasing the risk of PVD.
- High Blood Pressure: Hypertension damages artery walls, contributing to the development of PVD.
- High Cholesterol: Elevated cholesterol levels lead to plaque buildup in arteries, restricting blood flow.
- Family History: A family history of PVD or cardiovascular disease increases the likelihood of developing the condition.
- Obesity: Excess weight exacerbates other risk factors, such as diabetes and high blood pressure.
Diagnosis of Peripheral Vascular Disease
Early diagnosis of PVD is crucial for effective treatment and prevention of serious complications. Diagnostic methods include:
- Physical Examination: A thorough physical exam, including checking for weak pulses in the legs or feet.
- Ankle-Brachial Index (ABI): A non-invasive test that compares blood pressure in the ankle and arm to detect blockages.
- Doppler Ultrasound: This imaging test uses sound waves to visualize blood flow in the arteries.
- Angiography: An invasive test that involves injecting a contrast dye into the bloodstream and taking X-rays to locate blockages.
Treatment Options for Peripheral Vascular Disease
PVD treatment focuses on managing symptoms, improving blood flow, and preventing complications. Key approaches include:
-
Lifestyle Modifications:
- Quitting Smoking: Smoking cessation is the most crucial step in managing PVD.
- Regular Exercise: A structured exercise program, particularly walking, can improve symptoms and enhance circulation.
- Healthy Diet: A heart-healthy diet low in saturated fats, cholesterol, and sodium can help manage PVD and its risk factors.
-
Medications:
- Antiplatelet Agents: Medications like aspirin to prevent blood clots.
- Cholesterol-Lowering Drugs: Statins to reduce cholesterol and plaque buildup.
- Blood Pressure Medications: To control hypertension and reduce artery damage.
- Diabetes Management: Proper management of blood sugar levels to prevent further vascular damage.
-
Surgical and Other Invasive Procedures:
- Angioplasty and Stenting: A minimally invasive procedure to widen narrowed arteries and place a stent to keep them open.
- Bypass Surgery: Creating a detour around the blocked artery using a graft to restore blood flow.
- Atherectomy: A procedure to remove plaque from the artery using a catheter with a cutting device.
Complications of Peripheral Vascular Disease
If left untreated, PVD can lead to severe complications, including:
- Critical Limb Ischemia (CLI): A severe blockage in the arteries of the legs that can lead to ulcers, infections, and, in extreme cases, amputation.
- Heart Attack and Stroke: PVD increases the risk of cardiovascular events due to the underlying arterial damage.
- Infections: Poor circulation can lead to slow-healing wounds and an increased risk of infections, particularly in the feet.
Living with Peripheral Vascular Disease
Managing PVD requires ongoing care and attention to lifestyle and medical treatments:
- Regular Monitoring: Regular check-ups with your healthcare provider to monitor the condition and adjust treatment as needed.
- Foot Care: Due to the risk of sores and infections, maintaining good foot hygiene and inspecting feet daily is vital.
- Support Systems: Engage with support groups or counseling to help cope with the emotional aspects of living with a chronic condition.
Preventing Peripheral Vascular Disease
Prevention of PVD involves addressing modifiable risk factors and maintaining a healthy lifestyle:
- Quit Smoking: Smoking cessation is the most powerful preventive measure.
- Healthy Eating: A diet rich in fruits, vegetables, whole grains, and lean proteins supports vascular health.
- Exercise Regularly: Physical activity, such as walking or swimming, improves circulation and overall cardiovascular health.
- Manage Chronic Conditions: Keep blood pressure, cholesterol, and blood sugar levels within recommended ranges to reduce the risk of PVD.
Conclusion
Peripheral Vascular Disease is a serious condition, but with proper management and lifestyle changes, its impact can be significantly reduced. Early diagnosis and treatment are key to preventing complications such as critical limb ischemia and cardiovascular events. If you’re experiencing symptoms of PVD, consult your healthcare provider to develop a personalized treatment plan that suits your needs.
If you’re concerned about Peripheral Vascular Disease or need help managing your condition, don’t wait. Contact us today to schedule an appointment and start your journey toward better vascular health.